Over half of the global population meets the diagnostic criteria for at least one psychiatric disorder in their lifetime, and "comorbidity" (having multiple disorders simultaneously) is common. Does the traditional diagnostic boundary still hold? A recent study in Nature shows, for the first time, mapped the "genetic landscape" of 14 psychiatric disorders using 1.05 million samples, revealing that 66% of genetic risk stems from 5 transdiagnostic factors. This provides a direction for re-evaluating the diagnostic system and advancing drug development.
① Unprecedented sample size: Integrating 14 childhood/adult psychiatric disorders with a total of 1,056,000 cases, the average sample size per disorder is 165% larger than that of previous studies.
② Five core genetic factors: Obsessive-compulsive, Schizophrenia/Bipolar, Neurodevelopmental, Internalizing, and Substance Use factors explain an average of 66% of the genetic variance.
③ Cross-ethnic validation: The first systematic comparison of East Asian, African, and European ancestral populations, revealing high genetic consistency for some factors.
④ Brain cell type specificity: The Bipolar/Schizophrenia factor is enriched in excitatory neurons; the Depression/Anxiety factor is highly associated with oligodendrocytes.
What Do the Five "Transdiagnostic Genetic Factors" Look Like?
F1: Obsessive-Compulsive Factor: Anorexia Nervosa, Obsessive-Compulsive Disorder, Tic Disorder, Anxiety Disorder.
F2 :Schizophrenia/Bipolar Factor (SB): Schizophrenia, Bipolar Disorder.
F3:Neurodevelopmental Factor: Autism Spectrum Disorder, Attention-Deficit/Hyperactivity Disorder, Tic Disorder.
F4: Internalizing Factor: Major Depression, Post-Traumatic Stress Disorder, Anxiety Disorder
F5Substance Use Factor: Alcohol/Cannabis/Opioid/Nicotine Use Disorder, Attention-Deficit/Hyperactivity Disorder.
F5: Substance Use Factor: Alcohol/Cannabis/Opioid/Nicotine Use Disorder, Attention-Deficit/Hyperactivity Disorder.
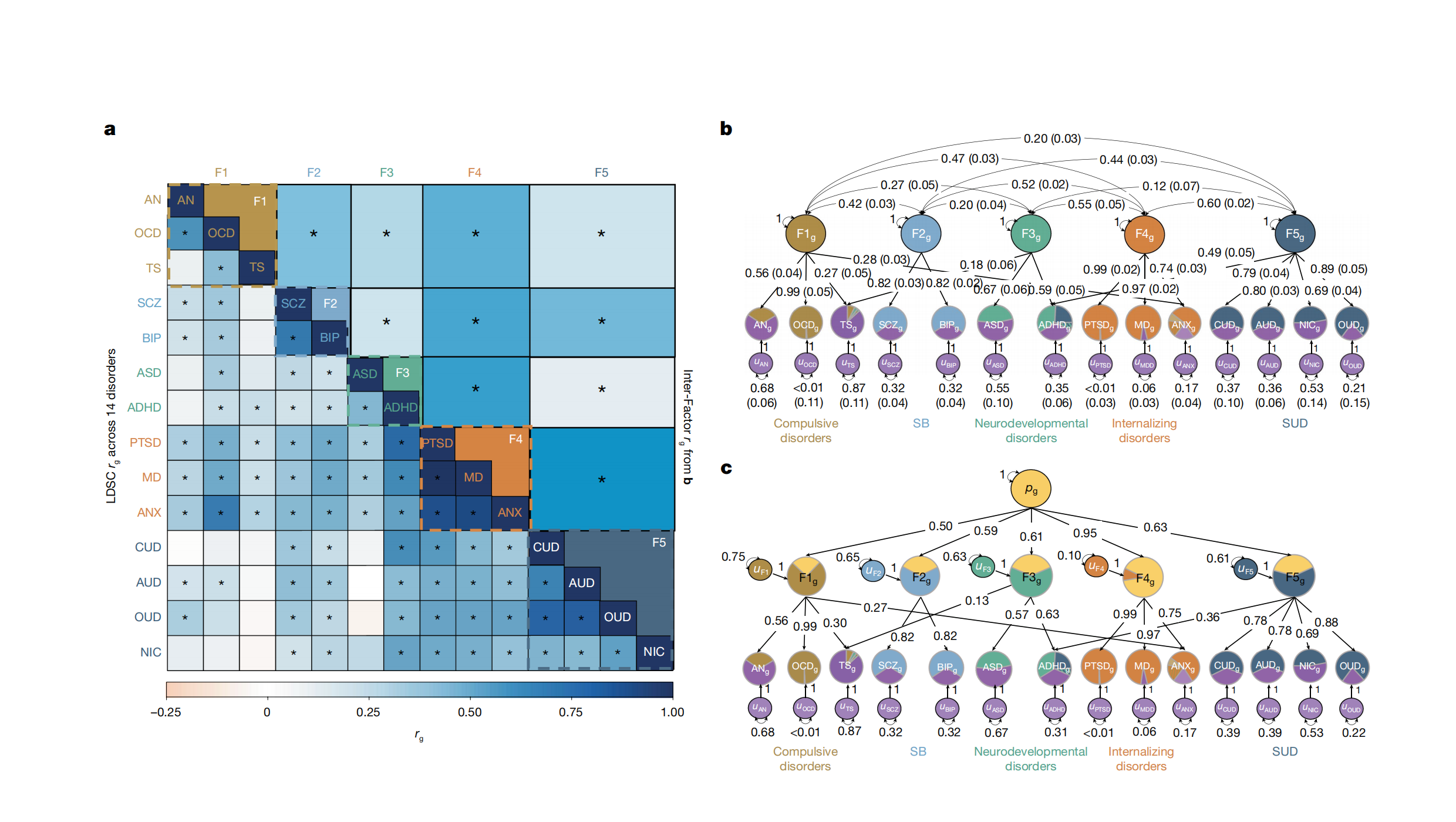
Figure 1: Five-factor model (Genomic Structural Equation Modeling) and heatmap of genetic correlations with external traits
Key Numbers
238 "broad-spectrum" risk loci are associated with ≥2 factors, accounting for 11% of all identified loci.
The NCAM1–DRD2 region on chromosome 11 is the "hottest" pleiotropic region, significantly correlated with 8 disorders.
The Internalizing Factor and Substance Use Factor have the highest genetic correlation (rg=0.60), indicating a biological basis for "mood-addiction" comorbidity.
Implications for Diagnosis and Treatment
Reconsidering diagnostic boundaries: Few "unique" genetic signals exist between Bipolar Disorder and Schizophrenia, or between Depression and PTSD/Anxiety, supporting a clinical spectrum perspective.
New drug strategies: Targeting excitatory neurons may address the excitation-inhibition imbalance shared by Bipolar Disorder/Schizophrenia; targeting oligodendrocytes may improve myelin plasticity in the Depression-Anxiety spectrum.
Repurposing existing drugs: Enrichment analysis of the five factors suggests that existing "broad-spectrum drugs" such as SSRIs and mood stabilizers already act on these transdiagnostic pathways.
"We provide a hierarchical model: at the top is a generalized psychopathological factor (p-factor), beneath which are five subfactors with greater neurobiological significance." — Corresponding author Jordan W. Smoller
Limitations & Future Directions
Primary data from European ancestral populations; East Asian and African samples remain small. Expanding cross-ethnic GWAS is needed.
Rare variants and gene-environment interactions have not been included. Future research can integrate whole-genome sequencing with longitudinal environmental data.
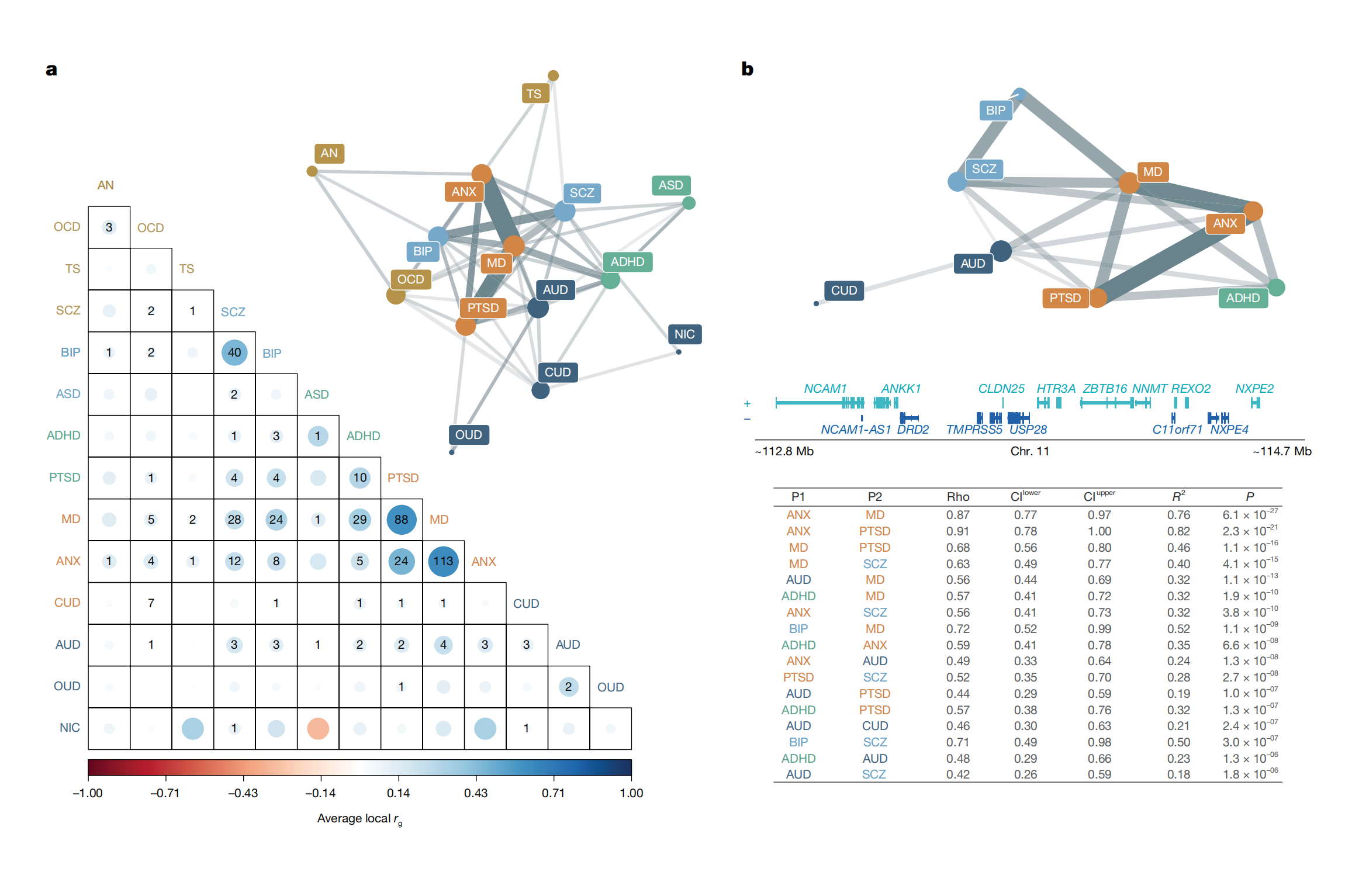
Figure 2: Local genetic correlations between the chromosome 11 hotspot region (NCAM1-TTC12-ANKK1-DRD2) and 8 disorders.
This article is based on the 2025 Nature paper "Mapping the genetic landscape across 14 psychiatric disorders".
Original article open access: https://www.nature.com/articles/s41586-025-09820-3
